Cariprazine is a new drug, a second-generation antipsychotic drug called by some authors a third-generation antipsychotic drug. It has been approved in the world in 2015 for the treatment of schizophrenia, manic and mixed episodes in the course of bipolar disorder. It is also useful in the treatment of depression in the course of bipolar disorder and unipolar depression [1].
The mechanism of action of cariprazine is complex. Its affinity for dopamine D3 receptors and action on 5HT1A, 5HT2A and alpha1B receptors differentiate it pharmacologically from other antipsychotics drugs [1]. Antipsychotics are generally thought to be effective against positive symptoms of schizophrenia, though they are less effective for treating cognitive deficits and negative symptoms associated with schizophrenia. Results from animal models suggest that the dopamine D3 receptor plays an important role in regulating cognition, mood, and social functions [2]. And partial agonism of the D2 receptors is responsible for the improvement in positive symptoms [1]. Most currently available antipsychotics have a lower affinity for D3 receptors relative to the very high affinity of dopamine itself for the D3 receptor that is why they do not occupy dopamine D3 receptors in the living brain. However, Cariprazine is unique among antipsychotics in that it has a higher potency for the D3 receptor than dopamine itself, meaning that the net effect of cariprazine administration is D3 receptor blockade [2]. Additionally, cariprazine has ten times higher affinity for D3 receptors than for D2 receptors, it induces an improvement in the elevation of positive, negative, and depressive (by attenuating chronic behavior with a lack of points), and it has a pro-cognitive effect. There are reports from studies on rats that partial agonism at D3 /D2 receptors, by reducing its effects on the reward system, may be the basis for the non-addictive effects of cariprazine [1].
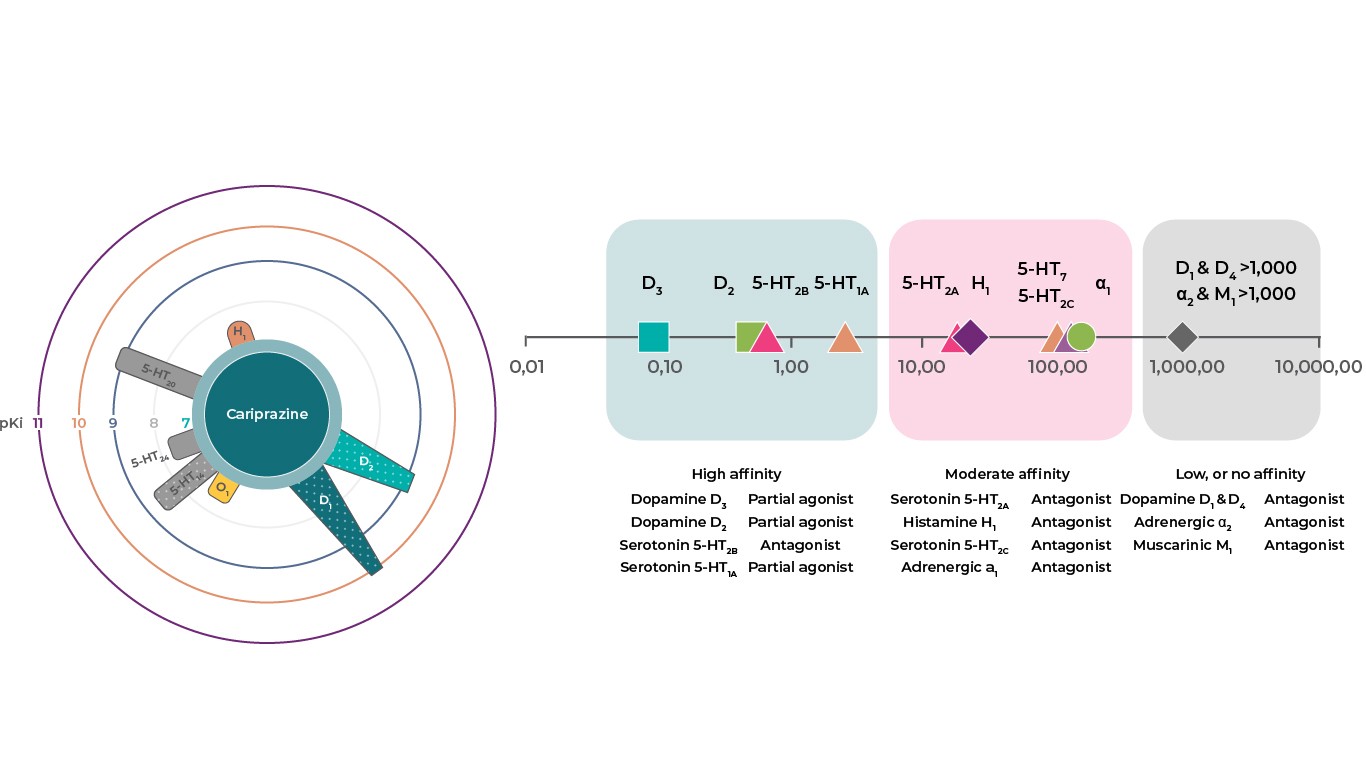
Partial agonism of 5-HT1A receptors is responsible for the improvement in negative and depressive symptoms, additionally, their stimulation is combined with the antidepressant effect of SSRIs and vortioxetine. Due to the antagonism of 5-HT2A receptors, there is a lower risk of extrapyramidal symptoms. As an antagonist of 5-HT2B and 5-HT7 receptors, it improves depressive symptoms and has a pro-cognitive effect. The antagonism of 5-HT2C receptors induces an improvement in depressive symptoms. Its partial agonism at dopamine D2 and D3 and serotonin 5-HT1A receptors, and antagonism of serotonergic 5HT2B receptors make it similar to aripiprazole and brexspiprazole. Finally, cariprazine exhibits partial antagonism at the histamine H1 receptor, muscarinic M1 receptors. However, due to its relatively low affinity for these receptors, its use is expected to carry a low risk of sedation, metabolic side effects or hypotension. High affinity for alpha 1B receptors is hypothetically associated with the reduction of extrapyramidal symptoms and actasia [1].
Thus, based on the mechanism of action and clinical studies, what additional applications and what will be the final position of cariprazine in psychiatry, will be shown only by our practical experience and post-approval studies on its effectiveness and safety. Perhaps cariprazine will also be used to potentiate the effect of antidepressants and in polytherapy of schizophrenia [1].
Source:
1. Rusinek, Adam, Gracjan Rudziński, and Jolanta Masiak. "New drugs in psychiatry-cariprazine, lurasidone, esketamine." Curr Probl Psychiatry 22.2 (2021): 2.
2. The mechanism of action of Reagila, available from: https://schizophrenialife.se/the-mechanism-of-action-of-reagila/?